By: Alix Cagnin, Emovi, Inc. R&D Engineer and Valerie G Wilson, Emovi, Inc. Clinical and Biomechanical Specialist ||

The knee is the most complex joint of the human body, and knee disorders account for a growing portion of visits to health care professionals1. While some of these disorders are preceded by a traumatic event (i.e., ligament injuries), other knee conditions, such as anterior knee pain and, more significantly, knee osteoarthritis (OA), progress and worsen over time in millions of people2. Conventionally, health care professionals are limited to radiographic and magnetic resonance imaging (MRI) as complementary tools to their clinical evaluation when diagnosing knee conditions. While these tools allow a proper assessment of the knee’s structural state at the time of the exam, they present several limitations, especially when assessing the risk of OA onset and progression.
Static imaging is limited, by definition, during weight-bearing activities and during loaded conditions, like walking. It is challenging for a professional to precisely identify when a knee problem began and determine what is causing stress to the knee joint. While these static assessments can help better understand the structural lesions around the joint, these results often do not change the initial diagnosis or medical decision-making. Furthermore, they may not provide optimal monitoring of the joint degeneration in shorter time intervals, as structural deterioration may plateau for several years even while the patient’s condition worsens. Indeed, this static information does not provide actionable data, as it is not well associated with the patient’s condition. Patients with mild radiographic OA often present with significant pain and functional limitations, while patients with severe radiographic severity may report minimal symptoms3. These limitations of static measures and the lack of actionable targets can be challenging for health care professionals when it comes to designing an effective treatment plan.
Knee disorders are often attributed to biomechanical dysfunctions4. Thus, dynamic biomechanical markers, which globally describe knee malalignment in the three planes of movement during walking (flexion/extension, adduction-varus/abduction-valgus, and internal/external tibial rotation), can provide relevant complementary information to static measures. These markers are linked to OA onset and are proven risk factors for disease progression5. For example, patients presenting with a varus thrust, a sudden lateral shift of the knee during the loading phase of the gait cycle, have more than two times the odds of incident and worsening medial bone marrow lesions, and 2-4 times the odds of worsening medial cartilage loss (i.e., joint space narrowing)5,6. The increased odds of these outcomes have also been reported with global movement alterations in the flexion-extension and varus-valgus planes.
Despite the added value of these markers in conjunction with information from static measurements, their assessment is often skipped in clinics due to the lack of validated tools and space to assess them with objectivity and precision7. Although static malalignment of the knee may be evaluated by traditional radiographs and MRI, these images do not capture the knee dynamic behavior, which is a central feature of the disease8.
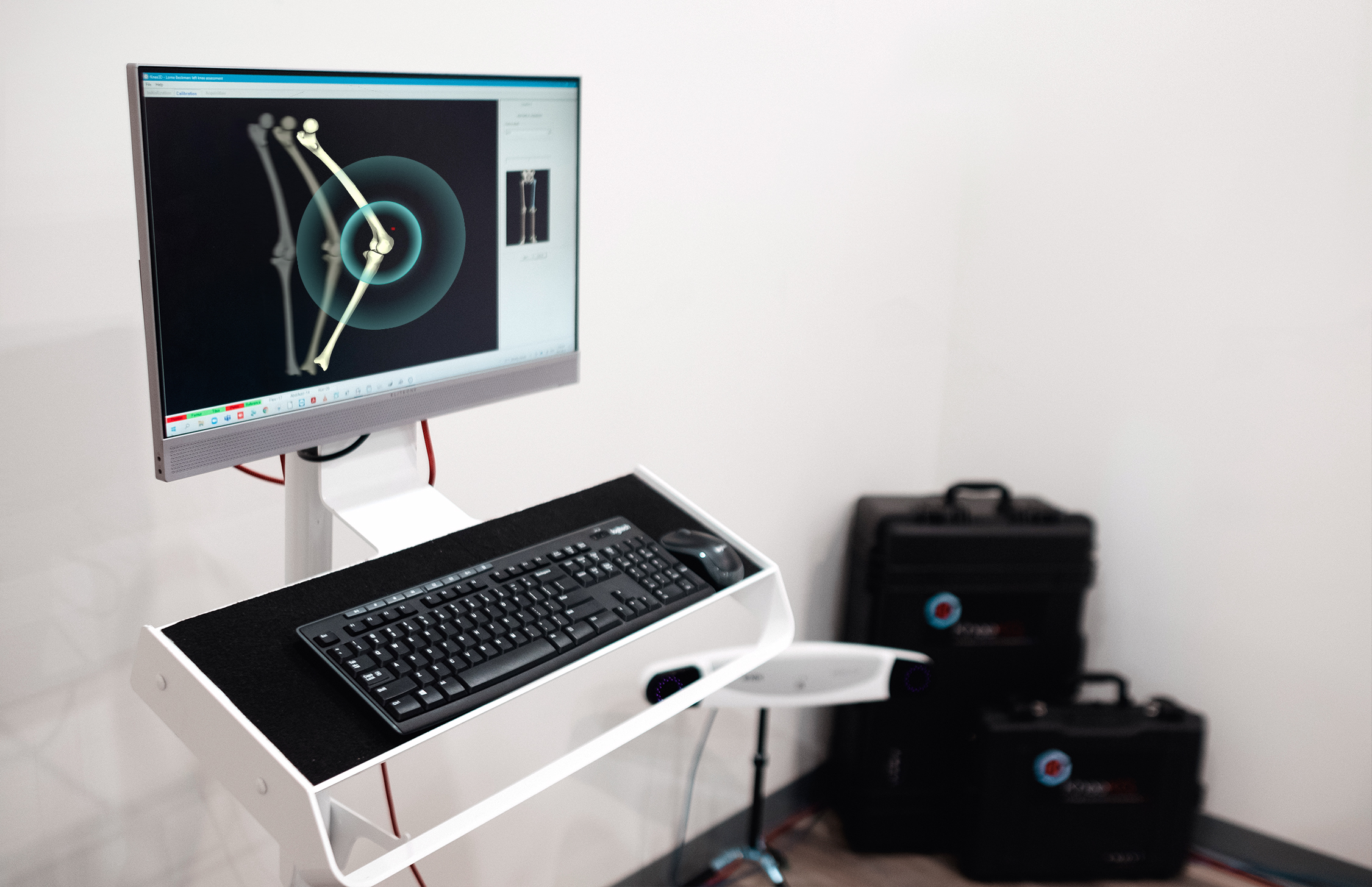
A Knee Kinesiography exam, which can quickly quantify 3D knee motion in a clinical context with patients walking on a commercial treadmill, constitutes a solution to this issue. It can be performed using the KneeKG™ system, a portable, validated, FDA (510K) cleared medical device manufactured and distributed by Emovi Inc. (Québec, Canada). It is comprised of a tracking device (exoskeleton) secured to bony landmarks on the patient’s lower limb and is designed to limit skin motion artifact. Thus, reflective markers fixed on the exoskeleton and tracked by an infrared camera system allows a precise real-time assessment of the knee joint motion rather than the skin movement9. Summarized information on biomechanical markers and deviations from what is considered a normal knee movement is generated by AI-powered solutions within the system. This easy-to-use exam can allow X-ray or MRI technologists to access new supportive data within 15 minutes and efficiently share this information with their referring physician to help them better understand the causes of their patient’s knee joint stress.
Dynamic biomechanical markers measured by a Knee Kinesiography exam are more associated with patient knee condition than static parameters measured on radiographs, which are descriptive of structural damage within the joint10. Numerous studies have shown that dynamic flexion contracture, malalignments in the varus-valgus plane, or excessive tibial rotation are largely associated with pain, function, and global health status in knee OA patients11,12. These associations support that this exam can be a valuable add-on for radiologists to complement available information for the diagnosis and to monitor, with more detail, the progression and impact of the disease. It can easily be included in the conventional toolset of health care professionals as users report reimbursement for this test using existing current procedural terminology (CPT) codes.
In addition, a crucial added value gained from the dynamic assessment of these markers is that, in contrast to static images (for example, joint space narrowing), they constitute actionable targets that can be addressed with personalized treatment recommendations. Recommendations include bracing and tailored functional exercises focused on the correction of joint malalignment and loading. Recently, the American Academy of Orthopaedic Surgeons (AAOS) and the American Association of Hip and Knee Surgeons (AAHKS) recognized the Knee Kinesiography exam in their updated guidelines for the clinical management of knee OA13. It was reported that an approach based on a Knee Kinesiography provides better patient education and targeted exercises with proven, better patients’ outcomes (i.e., significant improvement of symptoms, pain scores, and function during activity of daily living)14. This exam’s comprehensive and relevant data enhances patients’ education and empowers them to engage in more active care and management of their condition.
Beyond the conservative management of knee conditions, a new algorithm-based application uses this dynamic information to help physicians identify patients who are deemed appropriate to be referred to a knee surgeon15. The complementary use of both static and dynamic measures can optimize the decision process and facilitate data-driven triage for patients eligible or not for surgeries such as a total knee replacement. The Knee Kinesiography can be viewed as a valued and complementary assessment to be used in conjunction with traditional radiographs and MRI. It can refine diagnosis and further assist health care professionals in their decision-making process (i.e., primary care physicians report being twice as satisfied when having access to a Knee Kinesiography exam compared to other tools alone)14.
References
- Jordan KP, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord. 2010;11(1):144–10. doi:10.1186/1471-2474-11-144.
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020 Nov 26;29-30:100587. doi: 10.1016/j.eclinm.2020.100587.
- Zhang W, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis. 2010;69(3):483-89
- Egloff C, Huegle T, Valderrabano V. Biomechanics and pathomechanisms of osteoarthritis. Swiss Med Wkly. 2012;142:0. doi:10.4414/smw.2012.13583.
- D’Souza N, Charlton J, Grayson J, Kobayashi S, Hutchison L, Hunt M, Simic M. Are biomechanics during gait associated with the structural disease onset and progression of lower limb osteoarthritis? A systematic review and meta-analysis. Osteoarthritis Cartilage. 2021 Oct 29:S1063-4584(21)00941-9. doi: 10.1016/j.joca.2021.10.010. Epub ahead of print.
- Wink AE, et al. Varus thrust during walking and the risk of incident and worsening medial tibiofemoral MRI lesions: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2017 Jun;25(6):839-845. doi: 10.1016/j.joca.2017.01.005.
- Royal Australian College of General Practitioners. Guidelines for the management of knee and hip osteoarthritis. 2nd EastMelbourne, Vic: RACGP;2018.p.1–82.
- Larose, et al. (2019). Can total knee arthroplasty restore the correlation between radiographic mechanical axis angle and dynamic coronal plane alignment during gait? 26(3):586-594.
- Lustig S, Magnussen RA, Cheze L, Neyret P. The KneeKG system: a review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012 Apr;20(4):633-8.
- Bensalma F, et al. (2021). Musculoskeletal and biomechanical characteristics are better associated with knee clinical condition than radiographic severity in osteoarthritis patients. Osteoarthritis and Cartilage. 29(S1), S265–S267.
- Omori G, et al. (2016) Association of mechanical factors with medial knee Osteoarthritis: a cross-sectional study from Matsudai Knee osteoarthritis survey. Journal of Orthopaedic Science. Jul;21(4):463-468
- Bensalma F, et al. (2019). A multivariate relationship between the kinematic and clinical parameters of knee osteoarthritis population. Biomed Eng Online. 2019 May 15;18(1):58.
- American Academy of Orthopaedic Surgeons Management of Osteoarthritis of the Knee (NonArthroplasty) Evidence-Based Clinical Practice Guideline. Published 08/31/2021. https://www.aaos.org/oak3cpg
- Cagnin A, Choinière M, Bureau NJ, Durand M, Mezghani N, Gaudreault N, Hagemeister N. A multi-arm cluster-randomized clinical trial of the use of knee kinesiography in the management of osteoarthritis patients in a primary care setting. Postgrad Med. 2020 Jan;132(1):91-101.
- Mezghani, N., Dunbar, M., Ouakrim, Y., Fuentes, A., Mitiche, A., Whynot, S., Richardson, G., “Biomechanical signal classification of surgical and non-surgical candidates for knee arthroplasty,” International Symposium on Signal, Image, Video and Communications (ISIVC), 287-290 (2016)