By Mark Day, EVP of Research and Development at iRhythm |
The pandemic has left an indelible mark on heart health and technology. Many with both pre-existing conditions and new symptoms avoided healthcare facilities, which increased the need for remote monitoring devices for around-the-clock observation at home. At the same time, those who contracted the coronavirus may suffer longer-term heart issues. As a result, digital transformation in healthcare accelerated, and AI is changing the way physicians deliver cardiac care.
Catching up on Care
Heart disease is one of the leading causes of death in both men and women in the United States. Atrial fibrillation is one of the most common cardiac conditions, affecting potentially more than six million Americans. COVID-19 has exacerbated these issues. Early research – which is still being investigated – shows the virus may cause lingering effects on the heart.
For some, the pandemic set back heart surgeries and interfered with regular care. Now, there’s an imperative for patients and physicians to catch up. Medical-grade wearable devices can help close the gap by enabling remote monitoring, anytime and anywhere.
Enhancing Cardiac Health Through Wearables and AI
In general, diagnostic solutions have advanced rapidly in the last 20 years, but cardiac monitoring innovation has, until recently, experienced a slow pace of change. Many clinicians still use antiquated, cumbersome, and uncomfortable technology, such as the Holter monitor — which is often unable to detect common arrhythmias due to limited monitoring duration and poor patient compliance.
Recent digital advancements have created smart, wearable biosensors that allow healthcare professionals to offer patients a more comfortable and, in turn, extended monitoring experience. However, with extended duration comes considerably more data to curate, which requires sophisticated means of analysis that combine AI-based algorithms and human experts to accurately identify anomalies even as short as four errant heart beats out of the 1.5 million typically seen in a two-week period – literally “needles in the haystack” of patient data.
We note, however, that AI encompasses a broad scope of algorithmic approaches, including both machine learning and deep learning algorithms. A powerful point of differentiation between these approaches is seen in the chart below, which illustratively compares improvement in accuracy with additional data. While both improve with additional data, only deep learning has the validated capability to approach the performance of expert humans in curating ECG.
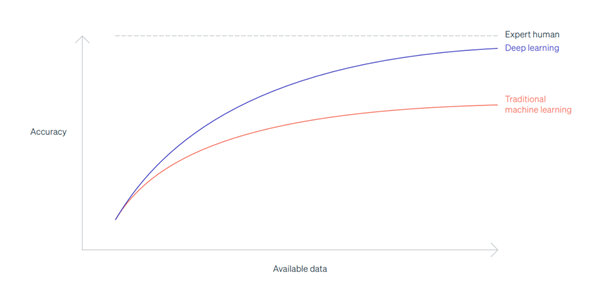 The combination of deep learning algorithms and expert human curation creates a trusted, scalable approach to identifying even minute anomalies in heart rhythms, which enables physicians to accurately diagnose and treat patients. Physicians can then focus on serving patients directly, rather than wasting time and healthcare resources retesting patients to capture the data necessary to make a definitive diagnosis.
The combination of deep learning algorithms and expert human curation creates a trusted, scalable approach to identifying even minute anomalies in heart rhythms, which enables physicians to accurately diagnose and treat patients. Physicians can then focus on serving patients directly, rather than wasting time and healthcare resources retesting patients to capture the data necessary to make a definitive diagnosis.
To enable these solutions, players in the digital health space must overcome numerous barriers. These include FDA regulation, which has been an obstacle for some health technology companies trying to operate in this space, particularly with respect to AI algorithms. However, with considerable investment into both verification and validation, regulatory clearance can be obtained. For example, iRhythm has recently implemented a second-generation of FDA-cleared, deep-learned algorithms for classifying and characterizing diverse heart rhythms at accuracy levels comparable to experts.
The Next Phase of AI Innovation in Healthcare
To this point, we have discussed the valuable application of AI – specifically deep learning – to the accurate analysis of recorded data. The next stage of AI is prediction: moving the paradigm of clinical insight from only retrospective reporting to also predicting risks about future conditions. The value proposition is clear: it’s more clinically meaningful to preventatively address and better manage future illness than to guide treatment and management of an existing illness.
In the healthcare sector, the key will be deciding who to monitor and when. With predictive capabilities, it isn’t just about mining patients’ retrospective data for anomalies, but also assessing all possible elements to identify who is at risk of a serious health event in future. Then, ensuring patients get the proper preventative medical care to prevent that health event from happening.
Researchers can look at previous conditions, genetics, drug use, ECG testing, and other factors to determine health patterns and anticipate outcomes. Employing AI will help to easily spot patterns and flag anomalies. Multiple inputs will be needed to identify risk and foresee potential impact.
This application of AI should also take external factors into account, such as population health and environmental conditions, and take a rigorous approach to ensure the data used to train the AI algorithms is both representative of the intended use population, and free from bias. Imagine, for example, having the capability to predict conditions that will affect a local community and preparing emergency departments with extra beds and staff ahead of time.
Digital technology such as AI is opening a new world of opportunity to enhance the patient experience, reduce the administrative burden on physicians, and improve health outcomes overall. Further adoption and advancements will undoubtedly transform cardiovascular care as we know it.
 About the Author
About the Author
Mark Day is the EVP of Research and Development at iRhythm. iRhythm is a digital healthcare company redefining the way cardiac arrhythmias are clinically diagnosed by combining wearable biosensing technology with cloud-based data analytics and deep-learned capabilities.