By Lucas Neff, MD, co-founder at Certus Critical Care |
For the acutely dying trauma patient, prehospital medicine is not enough, it must be precision prehospital medicine. This need is particularly pressing in the context of medication and fluid delivery to the patient. Methods to administer intravenous fluids have evolved very little over the last 100 years. Often, boluses of crystalloid and even blood products are given in standard amounts (e.g., 1 liter of saline or 1 unit of packed red blood cells) and crude measurements of response (heart rate, blood pressure and urine production) are intermittently assessed to determine a response. Because of this lack of precision, patients often receive excessive amounts of IV fluids early in profound shock, which can lead to pulmonary edema, coagulopathy, and even renal failure, all of which make prehospital care more difficult.
When crystalloids are insufficient to maintain blood pressure, the large doses of vasopressor medications that are then used can result in distal ischemia and the loss of digits and even limbs when used at very high doses. At present, medication administration is a cognitively demanding process that requires the clinician to accurately assess the type and dose of the medication and then manually deliver the drug into the patient. The ability to assess the effectiveness of the medication and then efficiently adjust and analyze the success or failure of those adjustments is extremely limited in austere conditions where environmental factors, fatigue, and medic experience all increase the potential for error. Moreover, the limited quantities of medications in resource-constrained environments make judicious medication selection and titration a high priority.
The Golden Hour from POI to Definitive care. Enter PACC-MAN
The advent of machine learning and adaptive/ “learning” algorithms to harness “big data” has created an environment where computers can interpret the complex physiologic signals from critically ill patients to provide nuanced second-to-second state predictions of ideal therapies. These advances have created opportunities to harness the power of robotics to help resuscitate patients.
The continued advancement in the miniaturization of processors and electronics have allowed for previously large form-factor devices to be miniaturized to allow for mobile applications. These advancements have allowed for complex processes requiring provider input and intervention, such as setting up an arterial pressure monitoring line or IV fluid/medication administration, to be easily automated and provided with minimal physical space and minimal power consumption.
The combination of advanced analytics, improved computing power, and medical devices capable of providing second-to-second interventions have ushered in the development of the next generation of critical care.
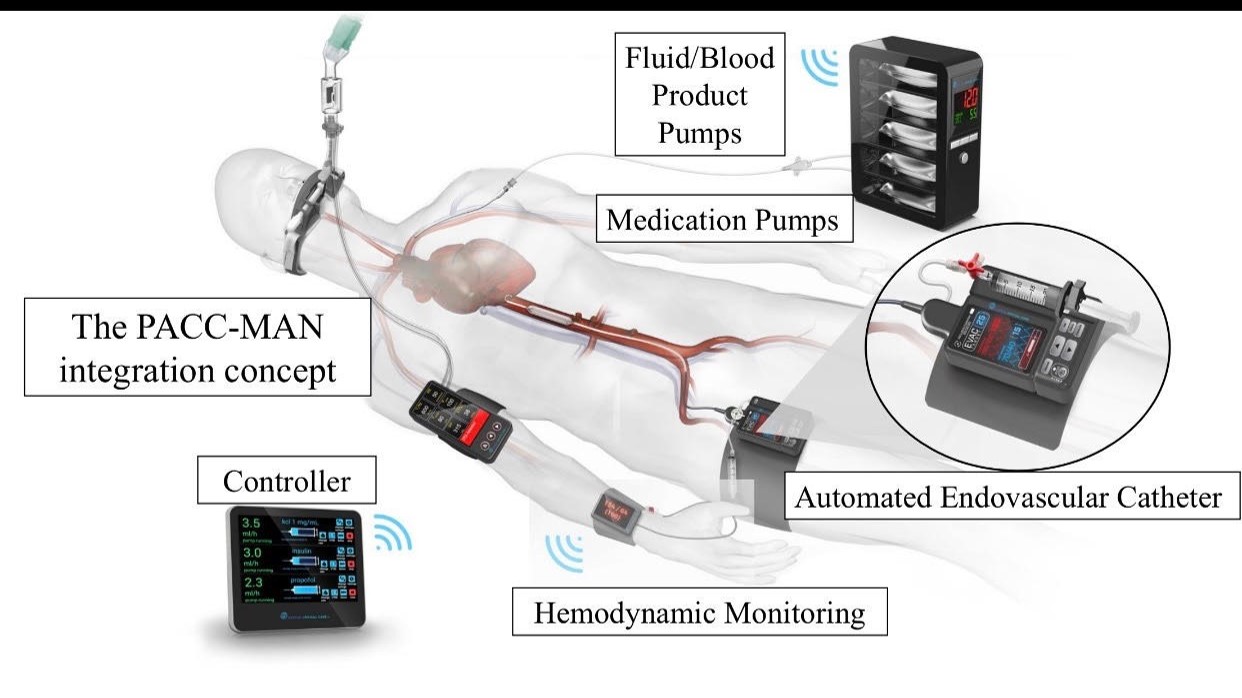
Partially Automated Critical Care Management (PACC-MAN) is the first platform of portable devices capable of providing nuanced critical care with minimal provider input. Two of the core tenets of critical care are IV fluid delivery and the use of medications that can directly improve blood pressure. The decision of when and how much fluid to provide and when to start blood pressure medications is a nuanced decision that currently requires repeated assessments at the patient’s bedside. This continual monitoring is difficult in the chaotic care environments of emergency departments and intensive care units.
The PACC-MAN platform uses advanced adaptive algorithms to identify when patients need IV fluids and or blood pressure medications and then autonomously controls peripheral devices to provide those therapies. By including physician-in-the-loop feedback of ongoing physiologic states, the PACC-MAN platform aims to extend the capabilities of current providers and assists in providing a tailored resuscitation for complex critically ill patients that would be impossible for a single physician to provide when caring for multiple patients at once.
Minimize interventions that don’t confer the real benefit – Why should you care?
Public Benefit: in the care of civilian trauma, particularly in rural communities where prehospital death is two-fold greater and in-hospital death is nearly four-fold greater as compared to urban centers. Soon, personalized, goal-directed critical care platforms capable of dynamically responding to changing physiology will decrease the material and cognitive requirements to care for critically injured patients and can greatly expand capabilities and improve outcomes in the prehospital setting and downstream- especially for rural trauma care with prolonged inter-facility transport times. The impact of automated critical care delivery is clear. Enabling lightweight teams (e.g., HEMS) with limited resources to bring advanced patient care techniques in austere environments will allow advanced lifesaving interventions to come to the patient.
The goal is to harness technological innovation to bring the best to the greatest number of patients. Taken together, smart resuscitation devices will revolutionize en route critical care and serve as force multipliers, distilling down the highly nuanced and complex critical care knowledge base for any medical provider in any environment. Furthermore, these technologies aim to limit the reliance on physical materials needed, not only fluids and medications, but also for ancillary equipment. If proven successful, this approach to personalized and adaptive critical care may represent a complete paradigm shift for the prehospital resuscitation of patients in shock.
 About the Author
About the Author
Lucas Neff is a former USAF general Surgeon and now is a pediatric general and trauma surgeon at a large academic medical center. He is a co-founder of Certus Critical Care, a medical device company leveraging the power of robotics for precision hemodynamic management. He can be reached at luke@certuscriticalcare.com.












