By Gretchen Zimmermann, RD, CDCES, Director of Clinical Dietetics at Vida Health |
 Type 2 diabetes is a chronic metabolic disorder that affects 34 million people — or 13% of the U.S. adult population. For people living with diabetes, physical and mental health is impacted by several psychosocial factors such as diabetes distress, depression, anxiety, eating disorders, low health literacy/numeracy skills, and limited financial and social resources — all of which can significantly impede successful diabetes self-management.
Type 2 diabetes is a chronic metabolic disorder that affects 34 million people — or 13% of the U.S. adult population. For people living with diabetes, physical and mental health is impacted by several psychosocial factors such as diabetes distress, depression, anxiety, eating disorders, low health literacy/numeracy skills, and limited financial and social resources — all of which can significantly impede successful diabetes self-management.
The ADA Standards of Care, 2021 recommends an HbA1c target of <7% without significant hypoglycemia for adult males and nonpregnant females with type 2 diabetes. Based on estimates between 2013-2016, among U.S. adults aged 18 and older with diabetes, only 50% meet this target HbA1c <7%, elevating their risk for complications. Although many people do live healthy lives, interventions to address barriers, achieve HbA1c and blood sugar goals, and reduce the risk of complications remain elusive for many.
Managing diabetes requires daily self-care to keep blood sugars in range so that therapeutic targets are met, quality of life is optimized, and the risk of long-term complications is minimized. Healthy coping skills are essential given the rate of depression in people living with diabetes, ranging from 9-34%, with diabetes distress affecting almost one-third of individuals.
Research published in Diabetes Care, 2020 suggests that clinical, psychosocial, and behavioral outcomes improve with initial and ongoing diabetes self-management education and support (DSMES). DSMES takes a care team approach to guide individuals in learning new skills, problem-solving, navigating daily self-care, setting personal goals, and coping with stressors. Barriers to receiving DSMES include accessibility issues (especially in rural areas), inconvenient class times or locations, cultural barriers, cost, lack of family support, lack of transportation, competing demands, and more. As of 2017, only 51.7 percent of adults aged 18 and over diagnosed with diabetes had received formal (DSMES).
So, how do we create accessible and practical solutions that address people’s self-care and psychosocial needs when living with diabetes?
Fortunately, technological innovations are creating solutions that address the myriad barriers that people face in managing diabetes. Patient-centered, digital health solutions that treat mental and physical health synergistically in a way that is accessible and scalable may lead to stronger outcomes — especially in those who are most in need of care.
The implications and costs of not meeting therapeutic goals
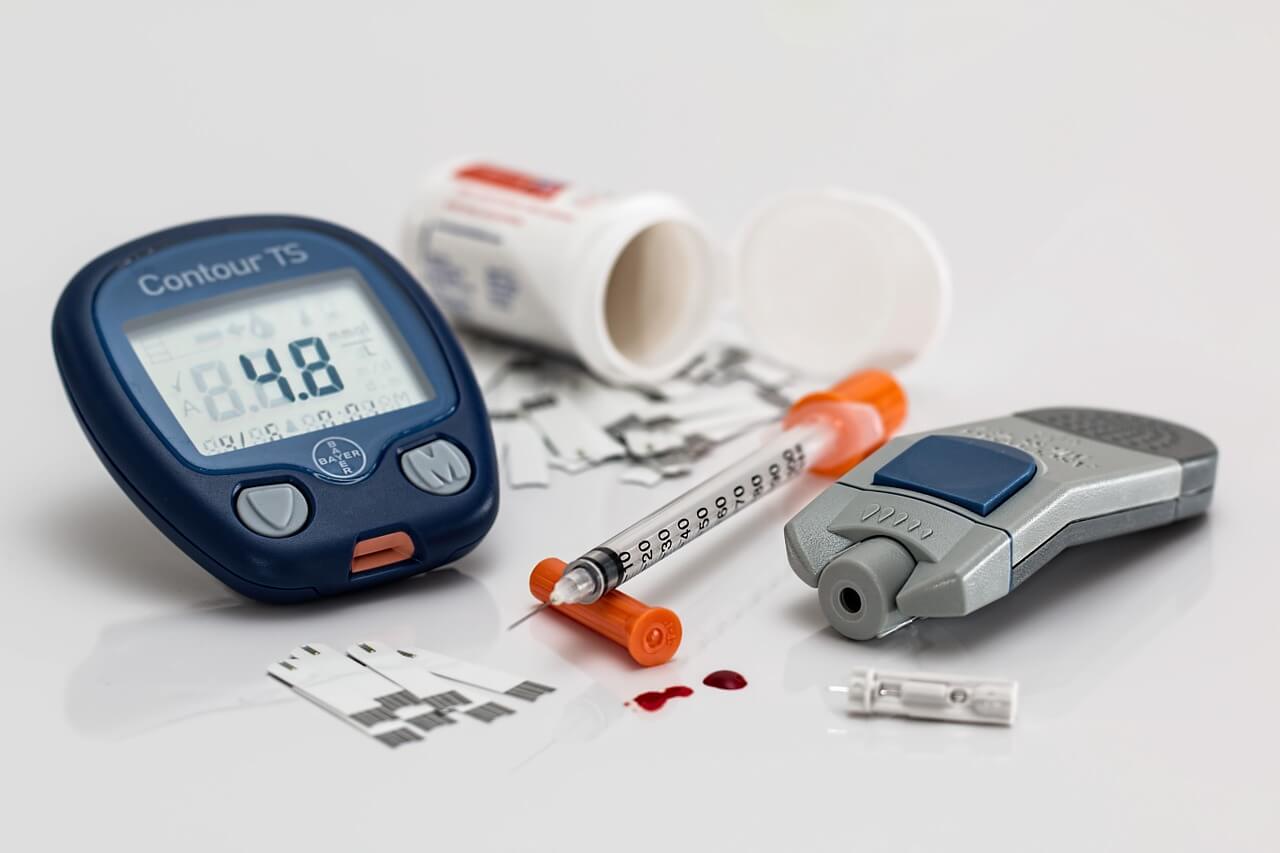
Managing blood sugars includes taking medications as prescribed, following an eating plan that keeps blood sugars in range, and self-monitoring blood sugar. Regular visits to a healthcare provider that includes HbA1c testing, screening, and preventative care, such as regular foot checks, are crucial aspects of diabetes care. Suboptimal diabetes management can have far-reaching health, economic, and financial implications.
Chronically elevated blood glucose can damage blood vessels and lead to long-term complications, including amputation, cardiovascular problems, vision loss, and kidney disease. Diabetes is an expensive disease, with medical expenditures being ~2.3 times more for people with diabetes than for those who don’t have diabetes. Associated financial costs were estimated at $327 billion in 2017, including $237 billion in direct medical costs and $90 billion in reduced productivity. The intangible costs like pain and suffering are also significant, contributing to a lower quality of life.

With half of the type 2 diabetes population not meeting therapeutic goals, we must ask, what are we doing wrong? Too often, advice like “exercise more, eat fewer carbohydrates, and take your medications” is overly vague and not helpful. Interpreting blood sugar data, reading labels, and calculating insulin doses are part of day-to-day diabetes self-care. Low health literacy and numeracy skills make self-care behaviors like problem-solving and treatment decisions more difficult. According to the CDC, “people with diabetes are nearly 2-3 times more likely to have depression than people without diabetes,” making healthy coping an essential part of diabetes care. The psychosocial barriers that people with diabetes face are complex and often require an interdisciplinary approach with varying degrees of expertise and support to be impactful.
Digital health solutions, like Vida Health, expand access to and increase utilization of diabetes management via a virtual environment. Diabetes experts and therapists are available to support physical and mental health. The combination of app-based functionality, personalized educational content, and one-to-one support from expert providers is a solution that improves clinical outcomes and, consequently, may lower health care utilization and costs.
The impact of psychosocial barriers on effective diabetes care
Psychosocial factors, including diabetes distress, depression, anxiety, eating disorders, low health literacy, numeracy skills, and financial constraints, can all hinder an individual’s ability to manage their diabetes successfully.
Diabetes distress and depression are associated with reduced quality of life and unsuccessful self-management behaviors, including taking medications as prescribed. Diabetes distress is an emotional response characterized by feelings of stress, guilt, and denial when facing the daily burdens of living with diabetes. According to a study published in Diabetes Care, 2010, individuals who experience depression have increased disease burden, greater severity of symptoms, decreased productivity, and increased use of health care services. Other studies have found a relationship between depression and hyperglycemia, which, when chronic, can lead to complications over time. One would be remiss not to mention the connection between mental health, eating disorders, and diabetes — with binge eating disorder being the most prominent eating disorder in people living with type 2 diabetes.
Low health literacy and numeracy skills, the ability to understand basic health information, and use numbers (data) to make appropriate treatment decisions are psychosocial barriers. Studies have shown that low numeracy skills are associated with less diabetes-specific knowledge and suboptimal blood sugar management. To accurately read and understand nutrition labels, understand serving sizes, and calculate insulin doses can all be challenging tasks for people with low health literacy and numeracy skills.
Mental health, physical health, and the many psychosocial factors are interconnected, with each having the potential to affect diabetes outcomes when not adequately addressed. Barriers exist in many settings that make screening for depression and diabetes distress challenging. Not all providers have the expertise or training to understand how to address social determinants of health — conditions in an individual’s environment that may impact health and quality of life. Comprehensive digital diabetes interventions that leverage providers’ expertise to effectively screen, triage, and treat are most welcome.
The role of an expert provider and digital health intervention in the management of type 2 diabetes
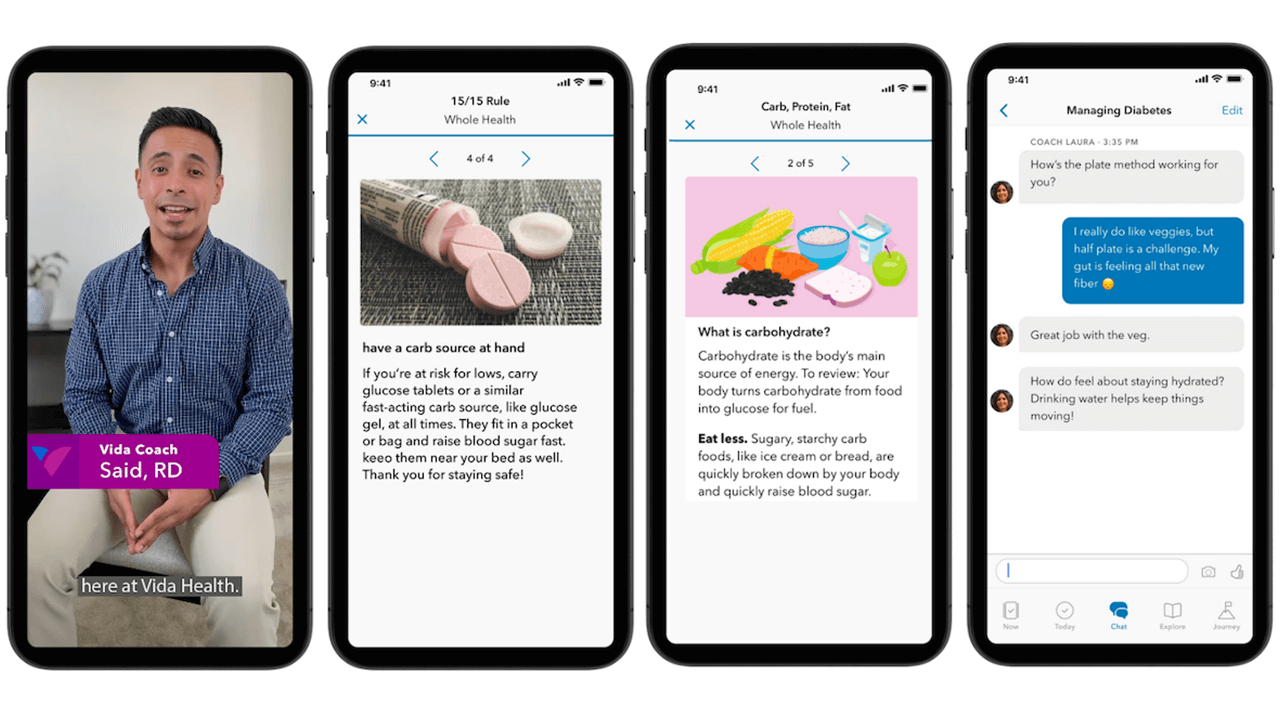 Research published by Vida Health in JMIR Diabetes, 2021, “Improved Glycemic Control With a Digital Health Intervention in Adults with Type 2 Diabetes: Retrospective Study,” revealed clinically meaningful outcomes in glycemic control among participants enrolled in a digital diabetes management intervention. Additionally, higher program usage was associated with more significant improvements in HbA1c compared to the group with lower program usage. The findings suggest that a digital health intervention paired with continuously available support may represent an accessible, scalable, and effective solution to diabetes management and improved HbA1c.
Research published by Vida Health in JMIR Diabetes, 2021, “Improved Glycemic Control With a Digital Health Intervention in Adults with Type 2 Diabetes: Retrospective Study,” revealed clinically meaningful outcomes in glycemic control among participants enrolled in a digital diabetes management intervention. Additionally, higher program usage was associated with more significant improvements in HbA1c compared to the group with lower program usage. The findings suggest that a digital health intervention paired with continuously available support may represent an accessible, scalable, and effective solution to diabetes management and improved HbA1c.
Diabetes experts, such as registered dietitians (RD) and certified diabetes care and education specialists (CDCES), partner with a person with diabetes to provide support and education. In doing so, they empower them to take charge of their health, promote self-efficacy, and teach strategies that support healthy coping while decreasing diabetes distress. Additionally, they help individuals deal with the daily emotional and physical burdens of diabetes through a motivational interviewing framework, specific and actionable goal setting using a patient-centered approach.
Trained experts can recognize when numeracy and health literacy challenges exist and help individuals overcome these barriers. They do so by using surveys to assess these barriers, providing education, using plain language, and teach-back methods to help improve diabetes knowledge. Over time, this can help build self-efficacy and motivation, creating a feeling of empowerment in one’s ability to take charge of self-care behaviors.
Recognizing when diabetes distress, mental health problems, and eating disorders co-exist or precede a diagnosis and escalating to a higher level of care when needed is critical. An interdisciplinary care model that creates a support system for the individual can set a patient up for success by helping them process health information and normalize the feelings associated with a new diagnosis or long-term management of a chronic condition. Lastly, using a patient-centered approach, where patient values guide clinical decisions, can indeed be a game-changer in a patient’s care.
Diabetes interventions, when enabled by technology and paired with expert support, are the future of diabetes care
Coordinated, holistic, and humanistic care combined with evidence-based interventions for people with multiple conditions continues to be the gold standard in patient care. From the moment a person is diagnosed with diabetes, and throughout their life, diabetes support and education should be made available to them in an easy-to-understand and accessible way.
Technological innovations, such as digital diabetes interventions that address the person as a whole, are making it easier for people to manage their diabetes and increasing access to care for a greater number of people living with type 2 diabetes.
 About the Author
About the Author
Gretchen Zimmermann, RD, CDCES, is a registered dietitian, certified diabetes care and education specialist, and Director of Clinical Dietetics at Vida Health. She leads a nationwide team of registered dietitians and diabetes experts in delivering best-in-class patient care through a virtual care platform. Gretchen is especially interested in the intersection of physical health and mental health, particularly related to patients with diabetes and other chronic conditions.
Published work: Zimmermann, G., Venkatesan, A., Rawlings, K. and Scahill, M., 2021. Improved Glycemic Control With a Digital Health Intervention in Adults With Type 2 Diabetes: Retrospective Study. JMIR Diabetes, 6(2), p.e28033.
Contact: gretchen@vida.com
About Vida Health
Vida Health is a virtual care platform intentionally designed to treat a person’s whole health by treating mental and physical conditions together. Vida’s clinically validated approach combines a personalized virtual care program that is anchored by the support and human connection of a nationwide network of coaches, registered dietitians, certified diabetes care and education specialists, and therapists. Vida’s app works with hundreds of connected devices, offers video sessions, asynchronous messaging, and digital content as well as programs to help people prevent, manage, and reverse chronic conditions — like diabetes and hypertension — and the mental conditions that accompany them — like stress, depression, and anxiety. Some of America’s largest employers and health plans trust Vida’s whole health offering. Learn more at www.Vida.com.












