Telehealth has been a lifeline for long-term patients throughout the pandemic — but what about those without reliable access to high speed internet?
By: Stephanie Wilding, CEO at CommunityHealth
COVID-19 sent telemedicine on the fast-track for widespread adoption, helping doctors manage and care for their patients — especially those at high-risk — during the nationwide shelter-in-place ordinance. But for patients in low-income families, there wasn’t such a simple solution.
While the ACA makes health insurance accessible for a significant number of Americans, there are still millions of vulnerable people who rely on receiving care from free clinics like CommunityHealth. So when COVID-19 hit the U.S. in March 2020 and strict shelter-in-place orders went into effect across the Chicagoland area, many low-income patients were left unable to seek basic treatment for their preexisting, ongoing, or newly-developed medical needs.
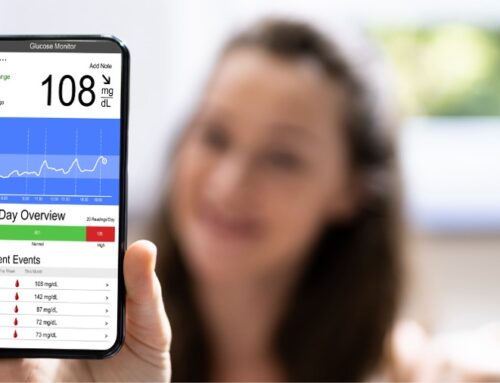
At CommunityHealth, the nation’s largest volunteer-based free clinic, we strive to deliver high-quality care to those who need it most, providing 15,000 medical and dental visits to thousands of Chicagoans who are underserved and uninsured each year. Up to 65 percent of our patients live at or below the federal poverty line, which is $24,300 for a family of four. Many also suffer from chronic conditions such as diabetes and hypertension, which require ongoing medical treatment.
While most healthcare providers turned to telehealth solutions to continue providing care to their high-risk patients during the pandemic, we knew that many of our low-income families wouldn’t be able to download additional software in advance of a virtual visit — a common prerequisite for many telemedicine tools — or even have reliable access to high-speed internet.
What we needed was a solution that worked with any smartphone as seamlessly as possible, and an easy-to-use telehealth solution that could be rapidly deployed across our network of providers. We also needed a simple platform for physicians and, most importantly, a user-friendly and accessible solution for our patients.
After evaluating several different telehealth solutions, we discovered many of our physicians were already Doximity members and had successfully adopted Doximity Dialer for virtual patient visits. Moreover, Dialer was made available to other healthcare professionals in the clinic’s network, enabling nurses and non-clinical administrative staff to coordinate with patients in a HIPAA-protected fashion.
“Being able to just open an app on my cell phone and securely call a patient when I am working remotely has been a game-changer,” said Babs Waldman, MD, a volunteer Medical Director at CommunityHealth. “I can call them using the clinic phone number instead of sharing my own private cell phone number. And they don’t have to take public transportation or find child care for their kids who are e-learning so that they can come to the health center for a check-in.”
Doximity Dialer proved to be an easy-to-deploy solution, especially for a volunteer workforce of
providers with a wide range of experience and comfort-levels with technology. Since many of our patients had limited access to conduct video visits via smartphone, Doximity audio calls helped mitigate issues with access to care, while maintaining both patient and provider privacy.
Once we got the solution fully implemented, we were able to clear a backlog of 300 patient visits, which had been postponed due to the pandemic. We’ve conducted nearly 4,300 telemedicine appointments, our no-show rates are down 24 percent, and virtual visits now account for 40% of all our medical appointments in 2020.
Our staff is relieved to be able to continue to serve our community and help low-income patients continue to receive the care they need, wherever they are.
About The Author:
Stephanie D. Willding, MPA (Steph) is a skilled healthcare and nonprofit leader, adept at developing and implementing transformative initiatives across organizations. Steph most recently served as Chief Officer of Strategy, Planning and Development at Chicago Family Health Center (CFHC) where she increased and diversified revenue, led data-driven performance improvement projects to expand access to care and improve quality outcomes, and advanced organizational goals through strategic and annual planning. Prior to joining CFHC in 2015, Steph was the Executive Director of the East Village Youth Program, a primarily volunteer-based youth services nonprofit. She holds a Master of Public Administration from the University of Illinois at Chicago, and a B.A. in International Studies from DePaul University.