Mercy’s COVID Care @ Home program plans to allow thousands of people with COVID-19 to have 24/7 access to a team of board-certified emergency medicine physicians who keep tabs on each person’s well-being via daily texts, video consults and phone calls. According to the company, the real-time, up-to-date medical advice for a quickly evolving disease has provided a safety net and kept patients out of the hospital at critical times when COVID-19 surged and hospitals needed all available beds.

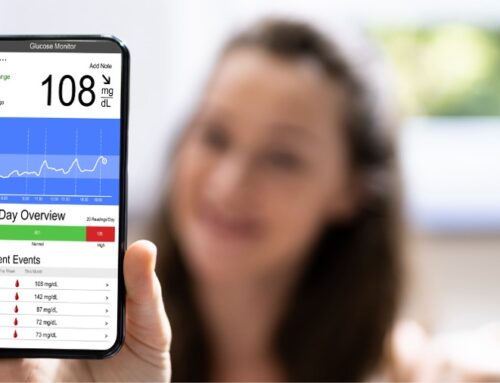
Pulse oximeters allow Mercy to closely monitor the oxygen levels of patients at home with COVID-19.
“It was scary how fast things changed for me,” said Christine Storm, 53, who tested positive for COVID-19 on New Year’s Eve. “My daughter flew home from California for Christmas. When she and her boyfriend landed in St. Louis, she found out they had been earlier exposed to COVID.”
Although they underwent numerous tests while in St. Louis, each family member’s results came back negative. The family carried on with holiday festivities but still used caution, limiting contact.
“As my daughter was flying back to California, she realized she couldn’t taste anything,” said Storm, a tax accountant. “I woke up that next day not feeling great. I did OK until the fifth or sixth day and then within 24 hours, I was really sick. In fact, two nights I woke up in the middle of the night and prayed I wasn’t going to die.”
Storm’s primary care physician referred her to Mercy’s virtual program.
“I couldn’t even go up and down the stairs because my oxygen levels had dropped so low,” Storm said. “Mercy monitored my oxygen very closely with a pulse oximeter. Mercy Virtual gave me a great amount of comfort in knowing someone was checking on me and I could reach out at any point of the day or night. They were extremely responsive.”
For Storm, the peace of mind was worth everything. Today she is fully recovered and back to work during a busy tax season.
To take part in the virtual COVID-19 program, patients are enrolled through a Mercy emergency department, urgent care clinic or primary care physician.
“This level of medicine is unheard of in virtual care,” said Dr. Justin Huynh, a primary care physician and vice president of population medicine at Mercy Virtual. “Mercy committed to staffing this program with board-certified emergency medicine physicians because they have the skill set and training to quickly troubleshoot in an intense and evolving situation. When you have something like COVID-19 and your condition can worsen in minutes, you want the expertise of an ER doc.”
Dr. Carter Fenton, an ER physician with more than 20 years of experience, agrees.
“We have created a 24/7 contact for these patients,” said Dr. Fenton, medical director of Mercy’s vAcute, a physician led team that cares for COVID patients at home, as well as addresses other acute care needs. “It’s real-time, high-level advice from a team of medical professionals who are experts in this dreadful disease.”
While some health systems have a virtual program that includes physician oversight, Mercy has a team of board-certified emergency medicine physicians on call around the clock
“That’s unique, and it can save your life,” Dr. Fenton said. “If needed, within 30 seconds, an ER doctor can hop on a call or video and troubleshoot best options with patients. And these are physicians who have been on the front lines with COVID and have seen the disease firsthand and know its many evolutions. What it might have looked like a week ago is different than what it is today. They have that kind of knowledge.”
Since November, the program has tracked more than 21,000 people who were able to recover from COVID-19 at home and 391 who were referred for a higher level of care when doctors determined their condition had worsened.
“Initially, people were going to the ER for any COVID symptom – shortness of breath, cough, you name it, but if they arrived and didn’t meet the threshold for being in the hospital, they were sent home. They were no better and they had no lifeline to expert medical advice like Mercy’s COVID Care @ Home,” said Dr. Fenton.
For most, Mercy’s COVID Care @ Home includes daily health checks via text. If the patient isn’t doing well, they can let Mercy know by responding to the daily text and activating an evaluation for another level of care – possibly a phone call, video consultation or even a visit to a clinic, ER or hospital if their condition worsens.
A patient with a Mercy physician can ask their physician to refer them to the program.