By: Dr. Waqaas Al-Siddiq, Chairman, CEO & Founder at Biotricity
Equal access to healthcare services is critical to achieving good outcomes – but many Americans still face barriers to receiving care. Healthcare disparities can be costly; there are approximately $93 billion in excess medical care costs and $42 billion in lost productivity per year as well as economic losses due to premature deaths tied to problems accessing care – and these healthcare disparities have only widened over time. Rural communities, elderly patients, and patients with disabilities or chronic illness may especially face difficulties in traveling to see providers. Telemedicine rapidly expands healthcare delivery to patients who lack ways to access traditional care and can significantly reduce these disparities.
Adoption of telemedicine accelerated during the pandemic as the need for remote care grew exponentially. Consumer adoption has skyrocketed, from 11 percent of U.S. consumers using telehealth in 2019 to 46 percent of consumers using telehealth now. This has led to big changes in reimbursement laws and FDA guidelines, which finally relaxed legislation that prevented physicians from practicing across state lines and to be paid the same for virtual visits as in-person ones. Some changes have been especially critical for increasing access to care: restrictions were lifted that limited services to rural patients, requiring them to travel to a healthcare provider before receiving a telemedicine visit, or only covering established patients rather than new ones. As transportation is a huge barrier to healthcare access for many, these changes may prove seminal in reducing disparities.
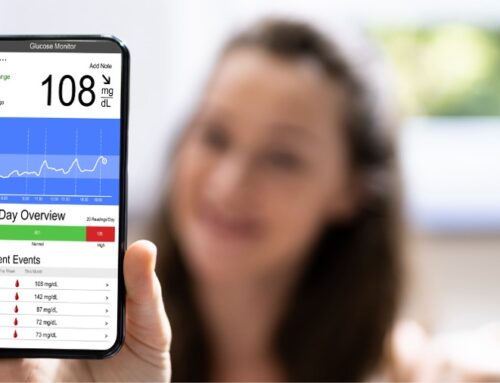
Now lawmakers are working to make these temporary changes permanent, opening more opportunities for virtual care. With the acceleration of telemedicine, we can expect to see more care shift from clinics to the home. With remote monitoring tools that allow physicians to track patient vitals and other biometrics, it’s now possible to outsource care previously done in a clinic – providing greater convenience for patients, and a reduction in cost for healthcare facilities. It’s also easier for patients with chronic conditions to be treated inside of their home, so they can continue go to about their daily lives while remaining engaged and in contact with a provider.
An estimated 84 percent of healthcare costs are attributed to the treatment of chronic disease, which is expected to grow in prevalence from 133 million in 2020 to 170 million in 2030. Rural communities have some of the highest rates of chronic disease and mortality rates, while rural hospitals are largely struggling financially and closing at a greater rate than ever before. This trend, along with limited access to specialty care in rural settings, exacerbates the access to care problem. Telehealth provides a unique opportunity to bridge this gap and implement preventative care that can stop costly readmissions and complications by increasing touchpoints with these patients.
Challenges to implementing telehealth still remain. Providers need to standardize education, for example, and make sure to provide training to healthcare workers who will be handling telehealth services on the job. For patients, it will be important to make sure that access to broadband is expanded, and that they have both cellular connectivity and devices that can support telehealth services. Medical device manufactures also need to improve integration with adequate connectivity – like 5G – to ensure high-speed data transfer and enable services like remote diagnostics. A study from Health Affairs in February found that telehealth usage during the pandemic was lower in communities with higher rates of poverty, revealing there are still disparities in access that need to be addressed.
And even though more than 96 percent of people in the United States own a personal cellphone, there are far fewer people that own smartphones, and that ownership varies greatly by age, race, education level, geographic area, and income. To address these disparities, some states introduced programs during COVID-19 to help provide smart devices to patients who needed virtual visits or monitoring. In order to bridge the digital divide and ensure that telehealth doesn’t leave some communities behind, more states will need to consider similar programs. It will also be important to work to improve digital literacy, which will affect telemedicine’s ultimate impact.
What can we expect for telemedicine’s future? In the near-term, we’ll likely see more virtual services tailored to address different population segments and conditions, and more robust specialty care options. More services will be able to reach patients directly in the home in the form of at-home lab tests, same-day prescription delivery, and at-home clinical trials. Soon, we’ll also see more advanced remote monitoring methods that will be able to collect additional biometric data for improved diagnostic capabilities, making preventative care for chronic conditions even easier. Telemedicine today is still limited in its capabilities, and its future will be integrating the areas needed to treat chronic patients better. Services like blood tests, remote diagnostics, medication adherence, and rehab programs will work together to create accessible at-home care programs.
In a post-COVID world, telemedicine utilization will decrease as some patients return to in-office visits, but the abrupt shift to remote care has kicked off a wave of innovation and continued growth is expected to continue for years to come. With its ability to reach rural communities, dispel traditional barriers to access, and facilitate preventive care, telehealth can help bridge inequities and reduce healthcare disparities. We’re just at the beginning of a digital transformation in healthcare, with telemedicine at the forefront.
About the Author
Dr. Waqaas Al-Siddiq, the founder of Biotricity, is a serial entrepreneur, a former investment advisor and an expert in wireless communication technology. Waqaas has a dual Bachelor’s degree in Computer Engineering and Economics, a Master’s in Computer Engineering from Rochester Institute of Technology, and a Master’s in Business Administration from Henley Business School. He also holds a Doctorate in Business with a specialty in Transformative Innovations and Billion Dollar Markets.