Lucienne Ide, M.D., PH.D, is the Founder and CEO of Rimidi, a clinical management platform dedicated to brining remote patient monitoring, chronic care management, clinical decision support, and patient reported outcomes together on one platform to improve workflows and patient outcomes. Recently, we had the opportunity to ask Dr. Ide a few questions about the current challenges that hospitals and healthcare organizations are facing.
1) With COVID variants causing rising transmission rates and hotspots around the country, what are some of the top challenges/pain points your customers are now facing as a result of the ongoing COVID pandemic and what role can technology play in mitigating such challenges?
The COVID-19 pandemic has shed a light on — and heightened — many of the challenges our hospitals and healthcare organizations have faced over the years, including the unsystematic way technology has historically been added and implemented to address urgent needs and move the needle towards value-based care. For example, as healthcare providers remain inundated with COVID-19 patients, they also are continuously running into tech roadblocks, including rigid electronic health record (EHR) solutions that cannot easily adapt to new and constantly changing workflows, as well as a lack of interoperability between various point solutions deployed under the guise of improving efficiency and quality of care. As a result, healthcare providers have been completely overwhelmed, with the majority of physicians reporting feeling burnt out and overworked.
In order to keep up with the rapid changes and challenges, such as limited resources and staff shortages, increased demand for services, and the inability to see patients in-person in many areas, hospitals and health systems quickly set up a number of niche technology solutions at the height of the pandemic, such as telemedicine platforms and remote patient monitoring (RPM) tools. These point solutions offered a bandage to help healthcare organizations stay afloat through the ongoing pandemic, and also helped with preventing hospital admissions and improving patient recovery from COVID-19.
With the pandemic continuing to strain hospital and health system resources, however, providers must take things a step further and evaluate all of the technology they currently have in place — and leverage new funding available — to achieve greater interoperability and flexibility designed to provide personalized, value-based care, and achieve overall population health goals.
2) You hit on point solutions being more of a bandage and less of a long-term strategy. Talk to us about how a platform approach enables greater workflow optimization and improved patient outcomes and engagement?
While point solutions like telehealth and RPM are extremely effective, it’s my opinion that they’ve only offered a bandage during the pandemic, and healthcare organizations are now realizing that many of these point solutions they quickly ramped up only addressed one particular issue.
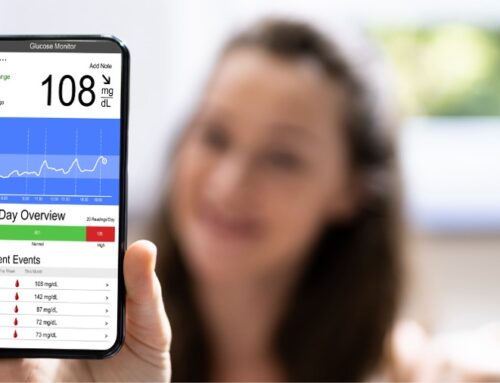
For example, RPM rapidly gained popularity at the onset of COVID-19, in part because of new flexibilities that made it easier for providers to get reimbursed for offering RPM. But it’s important to remember that RPM isn’t meant to just enable reimbursements. RPM codes, and other CPT codes added over the years like CCM, are meant to be an on-ramp to outcomes-based medicine by changing care delivery from episodic and always in-clinic to continuous and sometimes virtual.
You can’t achieve holistic chronic disease management without RPM, and RPM cannot be effective in achieving better outcomes if the patient-generated data isn’t made actionable with clinical decision support tools. That’s why hospitals and health systems should instead leverage a single platform in place of multiple disconnected point solutions, which enables them to provide individuals with the care they need, thus improving clinical workflows and driving better overall population health.
3) What components of care must be incorporated into such a platform to meet a health system’s new needs?
As providers continue to embrace technology as an enabler of more proactive, continuous care, they need an EHR-integrated composable digital platform that enhances the EHR for clinicians by adding clinical decision support and patient-generated data — either from connected devices or patient-reported outcomes surveys — to improve chronic disease management. Tying these powerful solutions together with a clinical management platform further enables holistic care of individuals by:
- Identifying patients who are not meeting standards of care
- Leveraging PROs and RPM to engage and empower patients to improve their health
- Driving greater efficiency for staff managing patients with chronic conditions
- Closing clinical gaps in care
Furthermore, by pulling together data from the disparate systems, these platforms can offer ongoing reporting, analytics and decision support that will help healthcare systems reach their clinical and operational performance goals. Only through such a multifaceted approach can providers achieve population — and individual — health goals and reach the pinnacle of value-based care for which providers have been striving for so long.
4) How does the Rimidi platform better support collaboration between practices or hospitals?
Our goal at Rimidi has always been to provide healthcare organizations with the innovative technology they need to optimize clinical workflows, enhance patient experiences, and achieve quality objectives.
Our recently enhanced composable digital platform is built to support various models of engagement and interventions for diverse patient populations, and empowers providers to move away from siloed point solutions. The result is that hospitals and health systems will experience greater workflow optimization and patients will receive improved outcomes and engagement.
Here are the specific ways in which our composable platform is used to deliver better workflows, experiences, and outcomes:
- Our SMART on FHIR integration to EHRs drives workflow efficiency for clinicians because it allows for rapid implementation, single sign on, and data exchange between Rimidi’s platform and the EHR.
- Embedded clinical decision support cards are easily configurable and mapped to national practice guidelines, protocols, remote monitoring alerts, and more.
- Chronic disease management is easier to deploy because of the comprehensive snapshot of cardiometabolic patients, allowing hospitals and health systems to better manage their population with multiple comorbid chronic conditions.
- Data from remote patient monitoring devices are combined with existing clinical data and weighed against provider and patient designated targets which are then used to drive clinical insights and actions.
- Quick questionnaires are easily sent to patients on their device in real time or in an event-driven context, and providers are able to view these responses and incorporate them into the clinical notes, allowing for more personalized patient care.
5) What must platforms do to secure patient data and privacy?
Protecting the security of patient data and privacy has become even more important, as the number of cyber attacks in healthcare has increased dramatically over the past few years.
There are a few best practices that platforms must follow in order to keep patients safe, which are outlined by the ONC. In working with EHRs, the first step is to make sure that the platform is HIPAA compliant, based on The Health Insurance Portability and Accountability Act (HIPAA) Security Rule, which “establishes national standards to protect individuals’ electronic personal health information that is created, received, used, or maintained by a covered entity, and requires appropriate administrative, physical and technical safeguards to ensure the confidentiality, integrity, and security of electronic protected health information.” The Security Rule has several types of safeguards and requirements which need to be applied, including administrative safeguards, physical safeguards, organizational standards, and policies and procedures.
Additionally, as a health IT platform, it’s important that when connected with the EHR, the following security features are included: ePHI encryption, auditing functions, backup and recovery routines, unique user IDs and strong passwords, role- or user-based access controls, auto time-out, emergency access, and amendments and accounting of disclosures.
In all, it is important to have strong cybersecurity practices in place to protect patient information, organizational assets, and personnel.
6) What are you most excited about for Rimidi and the healthcare industry at large looking forward?
At Rimidi, we’re excited to continue to demonstrate what is possible through an interoperability first approach and great product design. Our overall move to a more comprehensive platform approach is driven by the fact that patients are people with unique circumstances and challenges. We have to help their data (from multiple different sources) tell their story so that clinicians can make the best decisions guided by that data and the medical literature and evidence. We see the future of healthcare technology headed towards integrated and interoperable solutions.
In fact, the industry is beginning to understand that in order to have a meaningful impact on patients’ health and providers’ ability to care for their patients, disparate solutions need to work together in concert. Gartner recently noted that healthcare provider CIOs are shifting their architectural requirements to a platform paradigm, and projects that by 2023, 35% of healthcare delivery organizations (HDOs) will have shifted workflows outside the EHR to deliver better digital experiences.
Looking forward, as health systems search for new ways to improve their clinical workflow, they are also looking to a new type of digital care delivery platform that incorporates the Internet of Things (IoT), advanced analytics, artificial intelligence (AI), consumer engagement and the ability to integrate with the overall healthcare ecosystem, including health information exchanges (HIEs) and participation in accountable care organizations.
So, when leveraging our platform, for example, which ties together RPM, PROs, CCM and CDS functionalities, providers can achieve population and individual health goals for their patients, as well as reach value-based care goals.
 About Dr. Lucienne Ide
About Dr. Lucienne Ide
Lucienne Marie Ide, M.D., PH.D., is the founder and CEO of Rimidi, a cloud-based software platform that enables personalized management of health conditions across populations. She brings her diverse experiences in medicine, science, venture capital and technology to bear in leading Rimidi’s strategy and vision. Motivated by the belief that we can do so much better as individuals, in industry and society, Lucie left clinical medicine to join the ranks of healthcare entrepreneurs who are trying to revolutionize an industry.