Medical device firm Masimo announced the attainment of the CE mark under the European Union Medical Device Regulation for its LiDCO board-in-cable (BIC) module, opening up an advanced method of hemodynamic monitoring to healthcare providers in the European market.

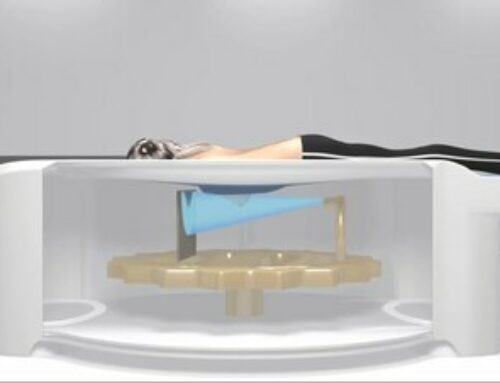
The LiDCO module is engineered to connect to multi-patient monitoring platforms, including the Masimo Root Patient Monitoring and Connectivity Hub, providing an enhanced hemodynamic monitoring solution. This development signifies a step forward by allowing clinicians to easily add LiDCO hemodynamic monitoring, which employs the distinctive PulseCO algorithm, to their Root patient monitoring hubs. Notably, the LiDCO module operates without requiring a dedicated hemodynamic monitoring box.
Moreover, the LiDCO module brings a broad spectrum of capabilities to the table, from potent guided protocols aimed at aiding the assessment of fluid responsiveness to providing detailed trending data and notifications for per-beat pressure analysis, which can be organized in the most beneficial configurations for each patient on the Root monitor. In combination with Masimo rainbow Pulse CO-Oximetry, the integration of LiDCO hemodynamic monitoring affords the potential to uncover noteworthy new insights into patient status.
The CEO of Masimo, Joe Kiani, expressed his enthusiasm, “By bringing LiDCO’s beat-to-beat advanced hemodynamic monitoring to Masimo Root, clinicians are now able to provide a more comprehensive, continuous view of cardiac output (CO) and oxygen delivery (DO2).” With the integration of Masimo’s noninvasive rainbow SET Pulse CO-Oximetry parameters and LiDCO’s innovative PulseCO algorithm, clinicians can continuously and simultaneously monitor various components affecting a patient’s oxygen delivery, such as cardiac output, stroke volume, pulse rate, total hemoglobin, and fractional oxygen saturation, alongside an automated estimation of DO2.
Designed for easy setup and versatile operation, the LiDCO module leverages a patient’s existing arterial line and blood pressure transducer to monitor numerous advanced hemodynamic parameters using the robust PulseCO algorithm. Its design aims to eliminate the usual delays experienced with other hemodynamic monitors, which often rely on assumptions about vascular compliance or detection of the dicrotic notch.
Dr. Max Jonas, a Intensive Care Medicine and Anesthesia consultant, highlighted, “The introduction of the Masimo LiDCO Module is clinically very exciting, as it will deliver dynamic hemodynamic monitoring, with a known documented positive impact on patient outcome.” While Dr. Daniela Chaló, MD, PhD in Neurosciences, underscored the LiDCO monitor’s several advantages in hemodynamic monitoring, she also noted its compatibility with various patient monitoring systems and the capability to help healthcare providers make better decisions.
Research has demonstrated the efficacy of LiDCO in reducing postoperative complications, costs, and even mortalities at 30 and 180 days after surgery in some cases. With the now CE-marked LiDCO module and its potential integration with Root, these technological advancements may render a new era in patient monitoring, elevating the care paradigm to further heights.
References
- Pearse R et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA 2014; 311(21):2181-90.
- Tengberg LT et al. Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg 2017; 104:463-471.
- Published clinical studies on pulse oximetry and the benefits of Masimo SET® can be found on our website at http://www.masimo.com. Comparative studies include independent and objective studies which are comprised of abstracts presented at scientific meetings and peer-reviewed journal articles.
- Castillo A et al. Prevention of Retinopathy of Prematurity in Preterm Infants through Changes in Clinical Practice and SpO2 Technology. Acta Paediatr. 2011 Feb;100(2):188-92.
- de-Wahl Granelli A et al. Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39,821 newborns. BMJ. 2009;Jan 8;338.
- Taenzer A et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010:112(2):282-287.
- Taenzer A et al. Postoperative Monitoring – The Dartmouth Experience. Anesthesia Patient Safety Foundation Newsletter. Spring-Summer 2012.
- McGrath S et al. Surveillance Monitoring Management for General Care Units: Strategy, Design, and Implementation. The Joint Commission Journal on Quality and Patient Safety. 2016 Jul;42(7):293-302.
- McGrath S et al. Inpatient Respiratory Arrest Associated With Sedative and Analgesic Medications: Impact of Continuous Monitoring on Patient Mortality and Severe Morbidity. J Patient Saf. 2020 14 Mar. DOI: 10.1097/PTS.0000000000000696.
- Estimate: Masimo data on file.
- http://health.usnews.com/health-care/best-hospitals/articles/best-hospitals-honor-roll-and-overview.