By: Don Godbee, Mobile Solutions Architect at Stratix
Telehealth and virtual care are not brand new phenomena suddenly cobbled together as a rapid response to the onset of the COVID-19 pandemic, but the average US patient could be forgiven for thinking that they are. Indeed, virtual visits to care providers and remote patient monitoring have been available for quite some time, delivering two key benefits:
- Providing a platform to address cost-efficiencies and accessibility to quality healthcare for the populace at large
- Playing a key role in managing a growing population of chronically ill seniors.
Prior to 2020, however, the rules of reimbursement and implementation for associated telehealth services were difficult to navigate, wildly differing at the state and federal level with a host of regulations further complicating matters. Federal reimbursement policies are centered on Medicare, via the Centers for Medicare and Medicaid Services (CMS) – the single largest payer for seniors and chronically ill patients. Additionally, compliance with the Health Insurance Portability and Accountability Act (HIPAA) dictated rigorous standards for direct and monitoring communications between care providers and patients. Complicating matters further, US states offered a patchwork of individual telehealth laws dictating separate Medicaid policies.
The result was a lack of clarity of how healthcare providers could overcome regulatory and financial reimbursement barriers to implement effective telehealth programs as well as a lack of parity in coverage services and payments for patients. To address this at the federal level, CMS released new guidance in 2020 to relax reimbursement restrictions for providers. Now, we’re at the cusp of a new era of telemedicine where providers could widely offer:
- Virtual office visits that address traditionally in-person services such as primary care, behavioral health and specialty care (e.g. pulmonary or cardiac health rehabilitation)
- On-demand virtual urgent care to address pressing concerns and urgently needed consultations
- Virtual broader home health services such as remote patient monitoring, outpatient disease management and various forms of therapy (e.g. physical, speech)
- Tech-enabled home medication administration helping patients receive injectable or consumable medication via monitored self-administration
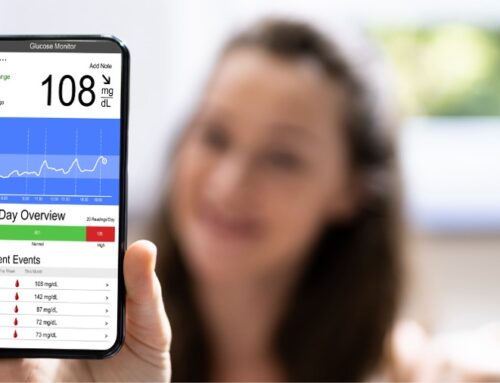
This is all, of course, dependent upon the mobile technology (e.g. tablets, wearables, etc.) and associated services that telehealth providers will rely upon to make these services happen at parity and scale for their patients. Even more importantly, virtual care programs being scaled up to cover a larger percentage of patients will fall apart if providers don’t have the resources to offer robust support and maintenance options for these devices and services. In short, quality of virtual care is highly dependent on persistent device and service availability and dependability.
Whether providers have already begun purchasing the mobile devices needed or are still struggling with the choice of what devices and services they need and/or can afford, however, they now face a different quandary: How to offer these virtual care services at scale in a sustainable way that works within current budget resources and doesn’t pass on ballooning costs to your patients?
One way to make complex mobile technology deployments financially manageable is opting for a mobile device as a service (mDaaS) model which shifts hardware from a capital expense to an operational expense spending model and allows telehealth providers to bundle or roll up a range of devices, accessories, services, maintenance and support into a single, predictable monthly per device price. With mobile device technology rapidly evolving, telemedicine providers will need the operational agility to pivot to different solutions and quick technology refreshes as the need arises. When done with the right third-party partner, mDaaS offers the additional advantages of outsourcing end-to-end support and lifecycle management to highly trained agents, who can free up precious IT resources. Most importantly, mDaaS creates a level of control over technology and spend that makes standing up virtual care programs convenient and stress-free.
There are many options to consider when expanding telemedicine services rapidly to larger patient bases, whether during disruptive events such as the COVID-19 pandemic or in the years to come. The key to making these services sustainable is finding a financing model that will free up internal resources, offer greater spending flexibility and offer end-to-end support for your healthcare mobile technology ecosystem.