By David Boucher, MPH, FACHE, Chief of Service Excellence at Aster DM Healthcare |

Telehealth became more widely adopted during the pandemic to expand access to essential health services. It helped reduce staff exposure to COVID-19, avoid surges in healthcare facilities and save critical resources like personal protective equipment (PPE). Additionally, there were reduced barriers to telehealth access and providers were able to deliver acute, chronic, primary and specialty care while improving patient health outcomes.
Many believe that the next 10 years may prove to be the decade when digital technology will reshape the health system. Strong continued uptake, favorable consumer perception and tangible investment in this space contribute to the continued growth of telehealth and digital solutions in 2021. In fact, new analysis indicates telehealth use has increased 38X from the pre-COVID-19 baseline.
The ability to maintain a continuity of care whenever possible is one of telehealth’s main benefits. Telehealth helps patients access primary care providers and specialists, including mental and behavioral health, manage their chronic health conditions and medications, assist with follow-up care after treatment and help with many other aspects of care.
Telehealth also benefits patients who opt for medical value travel (MVT) because it can provide initial conversations and post-operative follow-ups when patients are coming from far-off geographies and travel restrictions might not make frequent travel easy and much more.
Medical Value Travel During the COVID-19 Pandemic and Beyond
Until COVID-19 hit, global medical travel had been growing as an industry for the last few decades. Defined as the practice of seeking medical treatment and care in another state, region or foreign country, people travel to gain greater, more timely access to care, take advantage of procedures not available in their home country and save money. Pent-up demand for elective and sometimes needed surgery following COVID-19 will also prompt increased adoption. While tourism is an attractive aspect of medical value travel, it is certainly not the main driver of destination medical care.
According to the Centers for Disease Control & Prevention (CDC), the most common types of treatment include dental care, orthopedic surgery, cardiac and neurological care, cosmetic surgery, organ and tissue transplantation, fertility treatments and oncology treatments. Each year, millions of U.S. residents travel abroad for healthcare. More and more Americans are traveling for safer, high-quality care that is also cost-effective. In the reverse, U.S. doctors and hospitals are encouraging foreign patients to come to America for care and treatment.
With 71% of U.S. international travelers planning to travel abroad in 2021 and the global medical travel market expected to grow from $19.79 billion in 2020 to $21.93 billion in 2021, it is safe to say in the wake of COVID-19, international medical travel remains a top choice for those in the U.S. and Canada looking for cost-effective medical care.
Digital Health Enhances Medical Value Travel
Knowing that doctors are available for any questions gives a patient peace of mind and that’s why everyone has adapted to seeking care via telehealth during the pandemic. Medical value travel is going to undergo a massive change as result of this digital capability. Historically, medical travelers did not have the opportunity to meet the doctor prior to traveling for care, at least not on widely available HIPA-secure and HITECH-compliant platforms. That has changed and now everyone can have virtual consults with the doctor who is going to perform the procedure. Or even better, patients can shop for their doctors remotely before finalizing a care provider that they ultimately proceed with.
Similarly, when patients are back home, they can still reconnect and make sure recovery and recuperation is in line with what is expected. In some ways, COVID-19 has brought about this needed change and many healthcare organizations now place more emphasis on digital solutions such as telehealth. As consumer behaviors change and shift rapidly, healthcare organizations that offer medical value travel will continue to offer these digital health options to support ease of access to care and make people feel comfortable traveling for healthcare.
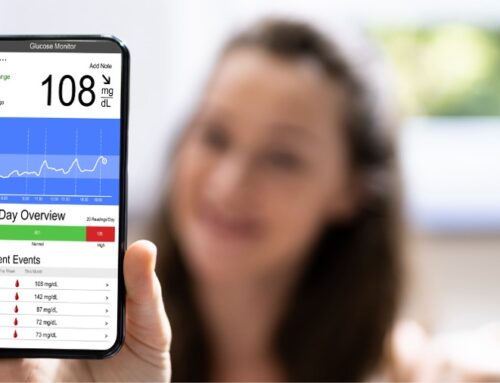
Access to healthcare can be significantly increased through innovative and digital methods like telemedicine, remote monitoring, E-ICU among others. With the availability of mobile networks, the initial consultation for medical value travel can take place through telehealth facility and the patients can visit the country only for a particular procedure. It is expected that this will be combined with leisure and wellness travel. Before the procedure, they can have online communications with their providers. Once the patient returns to his/her home country, follow-up can take place remotely. Distance is no longer a problem and patients can be evaluated, diagnosed, and offered treatment options through smartphone or video conferencing. They also use wearable technologies and measure biometrics. Other technologies include instant messaging apps, electronic records, and AI-enabled options.
In medical value travel, digital health tools can enhance communication and engagement between patients and their providers which can give easy access to transparent information, help them make informed decisions and get safe treatment. It can also build trust between the patients and their providers by having complete details in writing, including understanding patient needs, medical history collection, price quotes, customer expectations and aftercare protocols and procedures.
For medical value travel providers, some of the benefits of digital health, include market scalability which can improve their ability to grow and manage more of their patients’ demands, improve personalization and transparency so patients know exactly how they will be treated, who will treat them and how much they will pay. Digital health can also improve a provider’s operational efficiency which can help lower costs.
Several key technologies encompass digital health to improve patient care and outcomes outside of telemedicine. It includes data analytics which can be used to find which practices are better for improving a patient’s health and reducing overall costs. With the use of business intelligence tools as part of their digital health solutions, providers can make value-based decisions from the daily practices of doctors and staff.
Health Tech Challenges: How to Improve Healthcare No Matter Where It Takes Place
The turning point in healthcare will come when all providers can use the historical data of a patient from their ethnicity, social status, family medical history, lifestyle etc. and use this information to predict how the person’s health will look like combining all these details. This trend is gathering traction as health systems inch very close to this reality.
However, some major challenges for health technology, including digital health and how it relates to medical value travel, remain and need to be addressed soon for this shift to occur and improve patient health outcomes around the world.
It’s essential to create a larger vision to share data across the fractured continuum of care. This patient-centered model can include the role of shared care records, open systems platforms and EPRs comparing functionality, scalability, deliverability and data quality. This should entail wider dissemination within a trust, for example, of digital solutions that might be effective across several clinical teams, to optimize the use of facilities and infrastructure but also taking a more unified regional ecosystem approach, whereby clinicians and patients – safe in the knowledge of interoperability and ease of use – can find digital technology from multiple vendors in a single place.
This makes it difficult to achieve a holistic view of the patients’ health—which is an important factor in terms of the quality-of-care clinicians can provide. The industry is very complex and many of the solutions available on the market still don’t follow the domain standards for the exchange of health data. Technology vendors must support clinicians in making the right thing to do the easiest thing to do, now more than ever. Consolidating data from existing systems, and clinical insights drawn from that data, can play a big role here.
While digital health solutions have been adopted at groundbreaking speed to overcome the pandemic, the policy makers have struggled to keep up with the pace. The challenge will now be able to see how the quick fix solutions can be rebuilt into integrated workflows that benefit patient choice. There are tools to manage patient demand and improve self-care without removing accessibility, but these need more than technology. One of the main challenges facing healthcare is to build on the digital gains that we all saw during the first wave of the COVID-19 pandemic.
Technology providers should support health and social care services as they move from a provider-based service to integrated care systems to manage the needs of their population and transform services. There is also a big emphasis on supporting health and social care providers to address health inequalities while they meet demands with waiting lists at unprecedented levels. In addition, healthcare workers need to be ready – technically – to be well-versed and augmented with a non-clinical team to enhance capacity with technology. Shortages of nurses and doctors can be partially eased by making the systems smarter.
Actionable analytics are especially important in the healthcare sector where one wrong decision can have serious consequences for individuals and even entire communities. This is where advanced analytics mechanisms like AI can help make the data actionable. Datasets will grow and stored data will be more sophisticated and detailed. The more data you acquire and store in old-fashioned systems, the bigger a problem you may have in the future.
Lastly, investments into technology are not cheap. They are expensive investments and will need to ensure optimization of facilities and infrastructure to be able to enable the change; drive better clinical outcome and not allow for multiple duplications and failures in IT implementation which are costly affairs. For humanity’s best future, there needs to be a push to reinvent systems and processes.
 About the Author
About the Author
David Boucher has worked in healthcare for over 40 years and currently serves as Chief of Service Excellence at the corporate level for Aster DM Healthcare. In this capacity, he is guiding the 26-hospital chain through its service excellence journey. Prior to Aster, Mr. Boucher served for two years as Chief Business Transformation Officer at Bumrungrad International Hospital in Bangkok, Thailand. Mr. Boucher previously served 18 years as an executive of BlueCross & BlueShield of South Carolina. From 2006 through 2016, Mr. Boucher also served as President of Companion Global Healthcare, Inc. – the world’s only medical tourism facilitator owned by a major health insurer. Prior to 2000, David served as CEO at several hospitals in the U.S.
Mr. Boucher earned his BS degree from Slippery Rock University (PA) and a Master of Public Health degree (MPH) from the University of South Carolina; he has been named a distinguished alumnus by both institutions.
He has been quoted in over 250 newspapers and journals including The Wall Street Journal, New York Times, The Economist, U.S. News & World Reports. He has been interviewed on NBC Nightly News and Fox Business News. Mr. Boucher as delivered lectures on disruptive innovation in healthcare at Harvard Business School, Yale School of Management, and Harvard Medical School. He currently resides in Dubai, UAE.